Vein thrombosis: how to spot the warning signs
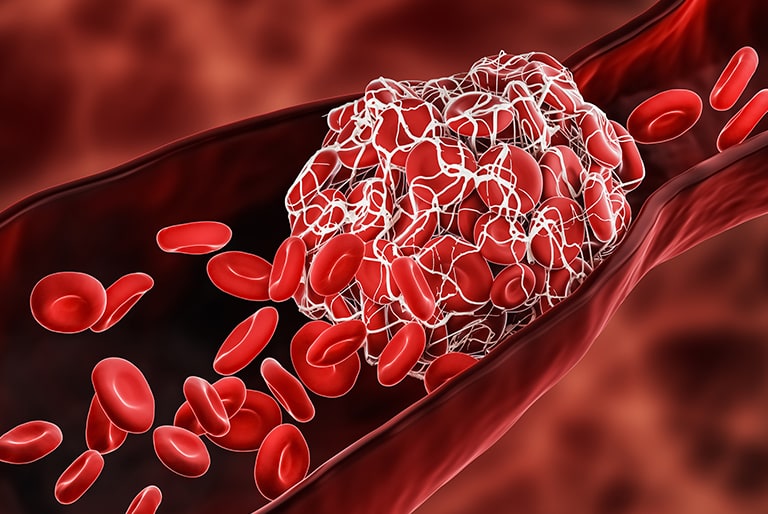
Vein thrombosis is something you must take seriously. If it is detected too late, it can cause consequential damage to your veins or even pulmonary embolism. Learn here how you can recognise thrombosis and how it can be treated.

What is vein thrombosis?
Doctors differentiate between two forms of leg thrombosis:
- Superficial vein thrombosis: if the blood clot develops in one of the superficial leg veins, e.g. due to varicose veins or vein inflammation, doctors talk of superficial vein thrombosis.
- Deep vein thrombosis: with a deep vein thrombosis (DVT) the blood clot develops in one of the deeper-lying leg veins. There is the risk of pulmonary embolism, which can be life-threatening and must be treated immediately!
What causes vein thrombosis?
Basically, anyone can suddenly get thrombosis. But there are some risk factors:
- Inactivity
- Prolonged sitting, e.g. in a car or plane
- Lack of fluids
- Excess weight
- Varicose veins
- Pregnancy
- Inflammation of vessels
- Coagulation disorder
- Heart failure
- Smoking
- Alcohol consumption
- Medication, e.g. hormone preparations, the pill
- Operations
- Increasing age
A healthy lifestyle with a balanced diet and regular exercise counteracts thrombosis, if not completely prevents it. People who remain seated for long periods, at work or when travelling, should integrate an exercise break every hour and stimulate the circulation in their legs.
What does thrombosis in your leg feel like?
A build-up of blood develops if blood can no longer flow through the vein due to the blockage caused by the blood clot. Thrombosis can be recognised by the following symptoms:
- Your leg swells up. Depending on where the thrombosis is located, your ankle, lower leg or even whole leg can become thicker.
- Your leg tightens and is painful.
- Your skin goes red or turns bluish and shiny.
- Your skin feels warm to the touch.
- Sometimes so-called “warning veins” are visible on your shin. They develop when your blood blazes another path through clear veins towards your heart.
You should consult a doctor immediately if these symptoms suddenly appear. Because if the blood bung detaches, it can be transported through the bloodstream into a vessel in your lung and cause pulmonary embolism.
If you have pains in your legs, accompanied by shortness of breath, coughing, palpitations, chest pain or even unconsciousness, you should call the doctor straight away! Until the doctor arrives you should follow the instructions given on the phone, stay calm and avoid any exertion.
How is vein thrombosis treated?
Early treatment is urgently required in order to diminish the risk on an embolism and to prevent further damage to the vein. There are several possibilities for this:
- Compression therapy: wearing compression stockings or applying compression bandages prevent the veins from expanding due to the external pressure. The pressure supports the flow of blood. Usually, after a case of thrombosis compression, stockings have to be worn permanently as part of the therapy.
- Medicines: anticoagulant medicines slow down the coagulation process and should prevent the thrombosis from growing. They are administered as a precaution after operations in the form of a Heparin injection, in order to reduce the risk of thrombosis.
- Thrombolysis: active ingredients which should dissolve the blood clot are administered by infusion.
- Operation: an operation is only necessary in the case of very severe vein thrombosis. The doctor removes the clot in an operation called a thrombectomy.
Can you have thrombosis without noticing?
Sometimes vein thrombosis produces no complaints at all and is symptom-free. It could also be that it only becomes noticeable after some time. Possible delayed effects of thrombosis are, for example, damage to the veins, venous insufficiency or functional disorder of the venous valves. Varicose veins can also be the consequence of vein thrombosis in your leg. That is why you should always take medical advice.
How can I prevent thrombosis?
Certain behaviour can reduce the risk of thrombosis, but not eliminate it totally. However, you can organise your day in a vein-friendly way:
- Exercise a lot: exercise keeps your muscle pump active, which conveys the blood out of your veins upwards towards your heart.
- Drink a lot: thick blood flows more slowly through your veins and so the consumption of ample amounts of fluids is important.
- Avoid long periods seated or standing: integrate regular exercise breaks for your legs and go for a stroll or do some foot gymnastics.
- Eat healthily: a balanced diet provides the vessels with an optimum supply of nutrients and counteracts excess weight.
- Do not smoke: nicotine damages vessels and thereby increases the risk of thrombosis and other vascular diseases.
- Wear compression stockings: anyone who has already had thrombosis should wear compression stockings as a precaution. They also reduce the risk of thrombosis on long journeys.
In addition to that, you can also support circulation in your legs with Veno SL® 300. The active ingredient it contains, Troxerutin, which is extracted from a substance from the Japanese Pagoda Tree, improves the fluidity of your blood and supports the walls of your vessels.